Can Gum Disease Be Cured?

Understanding Gum Disease
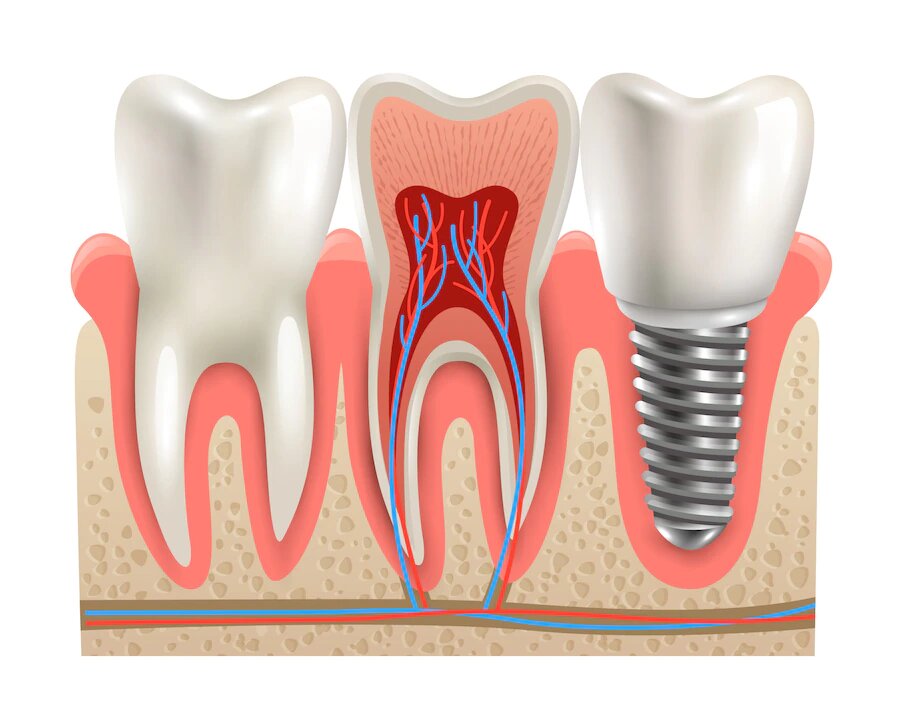
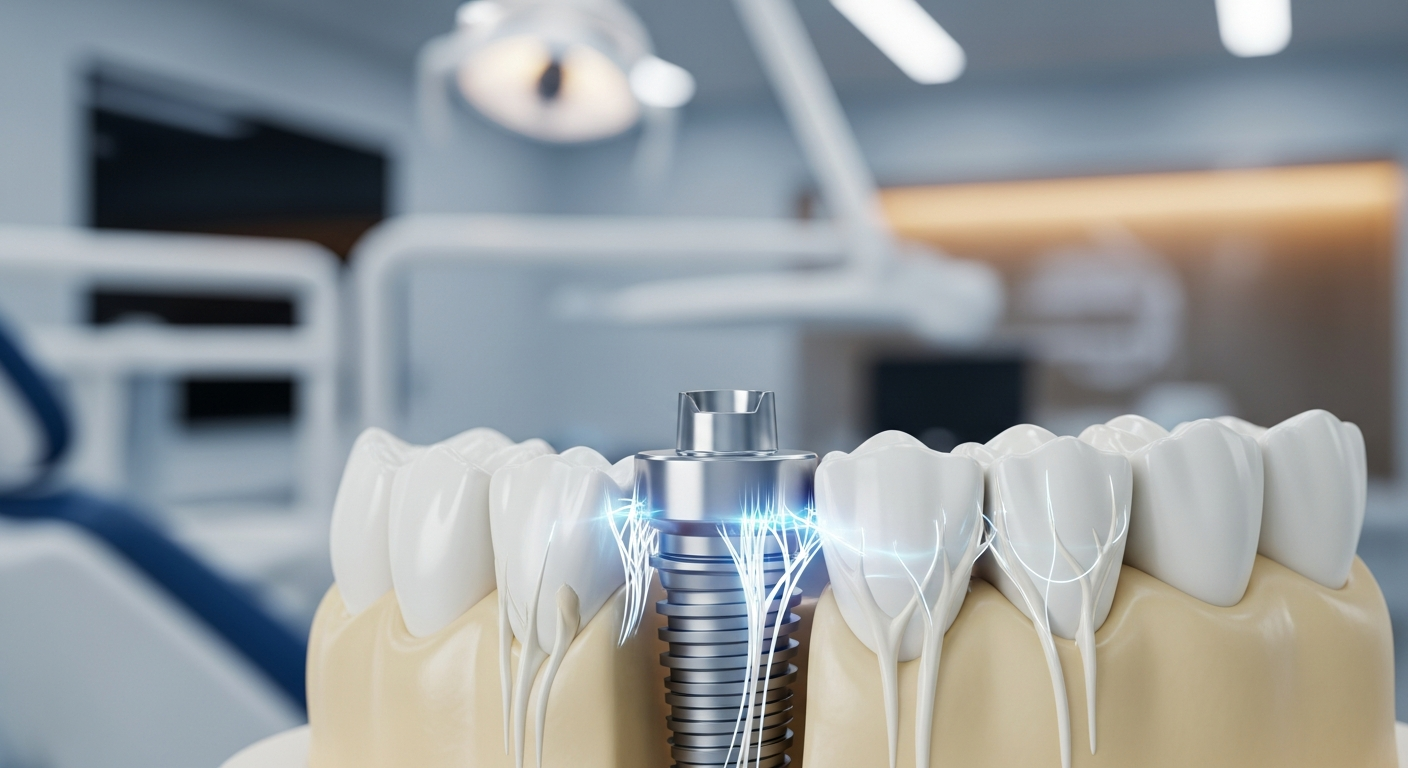
Gum disease, also known as periodontal disease, is a condition that arises from inflammation and infection of the gum tissues surrounding the teeth. It can lead to various dental complications if not addressed promptly.
Causes of Gum Disease
The primary cause of gum disease is poor oral hygiene, which allows plaque— a sticky film of bacteria—to build up on the teeth. When plaque is not effectively removed through regular brushing and flossing, it hardens into tartar, making it more difficult to clean. If left untreated, this can spread to the bones surrounding the gums, potentially resulting in loose teeth or the need for tooth removal.
Here are key causes contributing to gum disease:
| Cause | Description |
|---|---|
| Poor Oral Hygiene | Inadequate brushing and flossing lead to plaque buildup. |
| Hormonal Changes | Fluctuations, such as during puberty or pregnancy, can affect gum health. |
| Smoking | Significantly increases the risk of gum disease and lowers treatment success. |
| Certain Diseases | Conditions like diabetes or AIDS can compromise gum health. |
| Medications | Some medications can affect saliva production, which is vital for oral health. |
| Genetics | Family history can increase susceptibility to gum disease. |
Risk Factors for Gum Disease
Several risk factors can predispose individuals to develop gum disease. These include:
- Smoking: This habit not only increases the risk of gum disease but also diminishes the effectiveness of treatment (NIDCR).
- Hormonal Changes: Hormonal fluctuations in women, such as those occurring during menstrual cycles, pregnancy, or menopause, may make gums more sensitive and vulnerable.
- Underlying Health Conditions: Diseases like diabetes can impair blood flow to the gums or hinder the body’s ability to combat infections, enhancing the risk (WebMD).
- Genetic Predisposition: Individuals with a family history of gum disease are more likely to develop it themselves.
- Age: The incidence of gum disease increases with age, making regular dental visits critical for older adults.
Identifying these causes and risk factors is essential for understanding and addressing gum disease effectively. Maintaining good oral hygiene practices and visiting a dentist regularly can help mitigate these risks and detect gum disease at its early stages. For more details on prevention, refer to our article on what is gum disease and how can you prevent it?.
Symptoms and Diagnosis
Gum disease often develops silently, making awareness of its symptoms and appropriate diagnostic procedures essential for effective treatment.
Identifying Gum Disease
The symptoms of gum disease may vary in severity, but early identification is critical to prevent progression. Common indicators include:
- Red, swollen, and tender gums
- Bleeding gums during brushing or flossing
- Shrinking gums that may pull away from the teeth
- Loose, sensitive, or shifting teeth
- Pain while chewing
- Bad breath that does not go away with regular oral hygiene
Recognizing these symptoms promptly can lead to timely intervention and potentially prevent serious complications such as tooth loss. Early stages of gum disease, like gingivitis, can be reversed with improved oral hygiene and professional dental cleaning.
| Symptom | Description |
|---|---|
| Red and Swollen Gums | Inflammation of gum tissues |
| Bleeding Gums | Common during brushing |
| Sensitive Teeth | Discomfort or pain in teeth |
| Shifting or Loose Teeth | Indication of severe gum disease |
For more on the early indicators of gum concerns, see our article on early signs of gum disease.
Diagnostic Procedures
When gum disease is suspected, a dental professional will conduct several diagnostic procedures. These may include the following:
Clinical Examination: A thorough visual inspection of the gums and teeth is performed. The dentist checks for signs of inflammation, bleeding, and plaque buildup.
Periodontal Probe Measurements: The dentist uses a periodontal probe to measure the depth of the pockets between the gums and teeth. If the measurements exceed normal levels (typically 1-3 mm), it may indicate gum disease.
X-rays: Dental X-rays are utilized to evaluate the bone surrounding the teeth. This helps in identifying any bone loss associated with advanced periodontal disease.
Medical History Review: Understanding the patient's medical history, including any pre-existing conditions or medications, is essential, as these can influence gum health.
These diagnostic procedures are vital for determining the appropriate treatment plan. For further information on how dental professionals diagnose gum disease, check out our article on how dentists diagnose and treat gum disease.
Effective recognition and diagnosis of gum disease can greatly enhance the chances of successful treatment and help individuals understand if gum disease can be cured?.
Treatment Options
When addressing the question, "can gum disease be cured?", it's essential to consider the various treatment options available. These treatments can be categorized into nonsurgical approaches, surgical procedures, and the use of antibiotics.
Nonsurgical Treatments
Nonsurgical treatments play a significant role in managing gum disease, especially in its early stages. These therapies primarily aim to control bacterial growth and may include:
Scaling and Root Planing: This deep cleaning procedure involves removing plaque and tartar from above and below the gum line. This process also smooths the roots of the teeth, aiding in the prevention of future bacterial accumulation.
Antimicrobial Agents: The use of mouthwashes and toothpaste containing antimicrobial properties can help combat the bacteria causing gum disease.
Regular Dental Cleanings: Maintaining routine dental visits allows for professional cleanings that can help prevent the progression of gum disease.
The effectiveness of these nonsurgical therapies can vary based on the stage of gum disease, individual response to treatments, and overall health.
Surgical Procedures
For individuals experiencing moderate to advanced gum disease, surgical intervention may be necessary. One common surgical procedure is:
- Pocket Reduction Surgery (Osseous Surgery): This procedure involves making incisions in the gum tissue to remove deep-seated plaque and tartar. Surgeons clean the roots of the teeth and reposition the gum tissue to minimize pockets where bacteria can thrive. This procedure is critical for restoring supportive tissues and improving overall oral health.
Antibiotics in Gum Disease Treatment
Antibiotics play a key role in managing gum disease, particularly in conjunction with other treatment options. Various forms of antibiotics may include:
Topical Antibiotics: These are applied directly to the gums to target infection and inflammation.
Oral Antibiotics: In some cases, oral antibiotics may be prescribed to eliminate more widespread infections.
In addition to antibiotics, using dental products formulated with antimicrobial properties can enhance treatment effectiveness. Regular dental check-ups aid in early detection and prevent further complications associated with gum disease (WebMD).
For further information on oral health, consider reading about early signs of gum disease and what is gum disease and how can you prevent it?.
Preventive Measures
Preventing gum disease is crucial for maintaining oral health. Individuals can implement effective practices to reduce the risk of developing gum issues.
Good Oral Hygiene Practices
Good oral hygiene is the foundation of preventing gum disease. Proper brushing and flossing habits can significantly minimize plaque buildup on teeth. The following table outlines recommended practices for maintaining oral hygiene:
| Practice | Frequency |
|---|---|
| Brushing with fluoride toothpaste | Twice daily |
| Flossing | At least once daily |
| Using an antiseptic mouthwash | Daily or as directed |
| Replacing toothbrush | Every 3-4 months |
Research indicates that plaque not removed regularly can harden into tartar, which requires professional cleaning to eliminate. Daily oral care routines, combined with routine dental cleanings, can greatly enhance gum health.
Regular Dental Visits
Regular dental check-ups and cleanings are vital in preventing gum disease. Dental professionals can detect early signs of gum issues and provide necessary treatment before conditions worsen. The general recommendation is to visit the dentist twice a year for routine examinations and cleanings. Early detection allows for successful reversal of gum disease, typically in its initial stage (Marlborough Dentistry).
In summary, focusing on good oral hygiene practices and maintaining regular dental appointments can significantly reduce the likelihood of developing gum disease. For more information about gum disease, including its early signs, check out our article on what is gum disease and how can you prevent it?.
Managing Gum Disease
Effectively managing gum disease involves understanding the different stages and implementing appropriate treatment strategies. The two primary stages of this condition are gingivitis and periodontitis.
Reversing Gingivitis
Gingivitis is the early stage of gum disease, characterized by symptoms such as red and swollen gum tissues that bleed easily during brushing (Marlborough Dentistry). If diagnosed promptly, gingivitis can be reversed. It primarily affects the soft tissue without causing any bone loss, making it crucial for individuals experiencing early signs to seek intervention immediately.
To reverse gingivitis, the following steps are typically recommended:
- Regular Dental Cleanings: Professional dental cleanings can help remove plaque and tartar that contribute to gum inflammation.
- Improved Oral Hygiene: Diligent brushing and flossing can eliminate harmful bacteria that cause gingivitis.
- Routine Check-Ups: Regular dental visits ensure early detection and treatment of any gum issues.
By following these practices, individuals can actively reverse gingivitis and prevent progression to more severe forms of gum disease. For more details on early detection, visit our article on early signs of gum disease.
Managing Periodontitis
If gingivitis progresses without treatment, it can develop into periodontitis, a more severe condition that affects the support structures of teeth. This stage may result in painful abscesses due to the infection spreading beneath the gums, and it can lead to significant tooth loss in adults if left unmanaged.
Managing periodontitis often involves a combination of the following approaches:
- Deep Cleaning (Scaling and Root Planing): This procedure removes tartar buildup below the gum line and smooths out the tooth roots to help gums reattach.
- Antibiotics: In some cases, dental professionals may prescribe antibiotics to control bacterial infection and inflammation.
- Surgical Procedures: Advanced cases may require surgical interventions to restore gum health.
Regular follow-up appointments are vital to monitor the condition and make any necessary adjustments to the treatment plan. Continued commitment to oral hygiene practices can also help manage and halt the progression of periodontitis. For further insight into effective home strategies, see our article on treating gum disease at home.
Understanding and managing gum disease are essential to overall dental health. Early intervention and consistent care can help prevent severe outcomes, ensuring that individuals maintain healthy gums and teeth.
Link Between Gum Disease and Overall Health
Systemic Health Conditions
Gum disease is not just an oral health issue; it is increasingly being recognized for its potential connections to various systemic health conditions. Research indicates that the bacteria responsible for gum disease can enter the bloodstream, leading to inflammation throughout the body. This inflammation is linked to several serious health conditions, including heart disease, stroke, and diabetes.
People suffering from periodontitis, the advanced stage of gum disease, face a heightened risk of developing additional complications such as dementia and other significant health issues. Thus, understanding the impacts of gum disease on overall health is vital for individuals seeking to maintain their well-being.
| Systemic Health Condition | Connection with Gum Disease |
|---|---|
| Heart Disease | Increased risk due to inflammation linked to oral bacteria |
| Stroke | Higher likelihood associated with gum health status |
| Diabetes | Poor gum health can complicate diabetes management |
| Dementia | Increased risk in individuals with untreated periodontitis |
For more details on how gum disease can affect health, refer to our article on the long-term effects of untreated gum disease.
Importance of Managing Gum Health
Maintaining good gum health is crucial for overall health. Effective management of gum disease can significantly reduce the risk of associated health complications. Regular dental visits and proper oral hygiene practices are essential for preventing and treating gum disease. Early signs of gum disease, such as red and swollen gums or persistent bad breath, should not be ignored (WebMD). Recognizing these symptoms can prompt individuals to seek timely care which can hinder the progression of gum disease and improve one’s systemic health.
By taking an active role in managing gum health through preventive measures and seeking timely treatment, individuals can safeguard their overall health and enhance their quality of life. Comprehensive care includes good oral hygiene practices and regular checkups with dental professionals who can assist in diagnosing and treating conditions like gum disease effectively. For additional strategies related to gum disease management, consider reading about how to reverse early gum disease and how dentists diagnose and treat gum disease.















































.avif)










.jpg)


















.avif)


















.jpg)


